Beyond the lump: The long journey with breast cancer

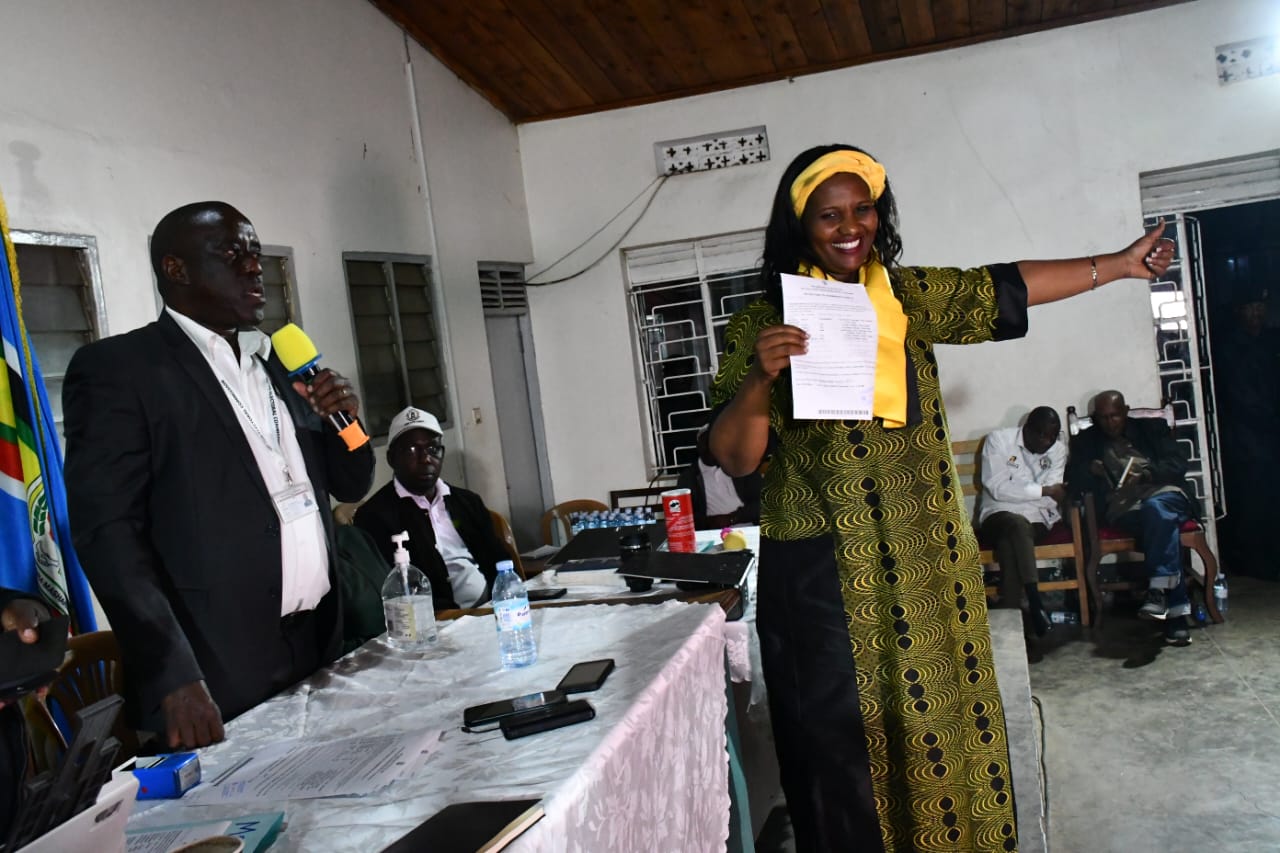
From L-R: Hilda Mwesigwa who has been cancer-free for 13 years since she completed her treatment, cancer survivor Denise Charity Atwine and Caroline Akello, whose breast was cut off. She had been diagnosed with stage IV breast cancer and underwent chemotherapy and radiotherapy. PHOTO/COMBO/COURTESY
What you need to know:
- According to the Global Cancer Observatory, in 2022 breast cancer was responsible for about 14.6 percent of all cancers in women and is the second most common cancer in women.
- An estimated 10 percent of breast cancer patients are men. As Beatrice Nakibuuka writes, breast cancer is responsible for about 6.3 percent of all cancer deaths in Uganda. It affects younger women in Uganda with diagnoses occurring between the ages of 30 and 50.
- Mammograms are the best tool for early breast cancer detection, and regular screenings can lower your risk of dying from the disease.
In 2018, Caroline Akello’s breast was cut off. She had been diagnosed with stage IV breast cancer and underwent chemotherapy and radiotherapy.
Two years later, when she went back to the hospital for a medical review, the doctors told her the cancer had spread to the spinal code and it was affecting her ability to lead a normal life.
“I was given a corset to wear because I had severe back pain. I could not do chores like mopping the house or lifting anything. Just when I thought I was getting better, my breathing worsened. The doctors told me the cancer was affecting my lungs,” she says.
Despite the bad news that comes with a stage IV cancer diagnosis, the thirty-eight year old has lived for over six years. Although she is on maintenance therapy, she is upbeat.
“For many people, a cancer diagnosis is a death sentence but I have a positive attitude towards life. I avoid negative people. I seek support whenever I can and I never miss the doctor’s appointment. As a single mother, sometimes, I forget that I have cancer because my daughter is my priority,” she says.
Women with breast cancer, especially those who have had mastectomies, do not feel attractive. Many are hesitant about having the surgery to remove one breast or both, and often shun treatment if that is the only option.
“People do not know about cancer. All they know about it is when they hear that someone has died from it. It is also expensive to travel from one’s home to Mulago Hospital regularly. I chose to get general treatment so I did not pay for chemotherapy. However, I paid some money for radiotherapy,” Akello says.
Expensive treatment
Uganda Cancer Institute (UCI) stands as a beacon of hope for many women seeking advanced care and treatment for breast cancer. Equipped with a specialised oncology unit, the hospital offers diagnostic services, including mammograms and biopsies. However, the demand often outstrips the supply.
For instance, UCI’s new radiotherapy machines require expensive and frequent maintenance. For this reason, the cost of radiotherapy treatment is very high, ranging from Shs800,000 to Shs1.8m. Tests, including a computed tomography (CT) scan, at UCI can cost about Shs500,000. In private hospitals, though, the tests can cost up to Shs800,000.
To the ordinary Ugandan, these costs may be prohibitive and are the reason why cancer sufferers delay in seeking medical care. Some resort to herbal remedies, which aggravate the disease since it keeps on spreading.
Services at UCI’s imaging centre for breast and prostate cancer are free, however, the number of those seeking services is always high. Some are late referrals from private hospitals or regional referral hospitals.
Denise Charity Atwine, a cancer survivor and patient navigator at UCI says the number of cases overwhelms the doctors.
“Education about breast health is improving but our facilities are thin on the ground. Women often wait for weeks to keep doctors’ appointments and many are unable to afford the costs of diagnostics, let alone treatment,” she explains.
Treatment options include surgery, chemotherapy, and radiotherapy. While UCI is making strides in expanding access to these services, barriers remain.
“Patients come from their homes with the attitude that they are in pain and need immediate attention, which they cannot get because of the numbers. This, therefore, leads to a retarded communication between the doctors and patients,” Atwine says.
Akello laments the cost of her treatment and the inconvenience it caused to her life.
“I had to travel several times from my home in Mukono district to UCI in Kampala. Each trip was exhausting and expensive. I had to find a modest place to stay in Kampala to reduce the transport burden,” she says.
The challenges multiply for rural women. Limited access to health facilities means they must travel long distances to receive care, often at great personal cost. Additionally, stigmas surrounding breast cancer can deter women from seeking timely treatment, leading to despair and isolation.
“After my breast was removed, it took me a year to look at myself in the mirror.
“Many husbands refuse to give their consent for mastectomies. Some patients at UCI are defrauded because language barriers make it hard for them to trace the right doctors. That is why patient navigators are important because they have survived the disease and know how to find their way in UCI,” Atwine says.
Over 80 percent of women presenting for breast cancer treatment at UCI have late stage disease attributable to a dysfunctional referral system and lack of recognition of early signs and symptoms among primary healthcare providers. Cancer treatment facilities are concentrated in urban areas, particularly Kampala City, leaving women in rural areas without necessary care.
Awareness of breast cancer symptoms and the importance of self-examination are gradually improving, yet remain low in rural areas. Screening programs, such as clinical breast examinations and mammography, are also limited, leading to late-stage diagnoses.
Barriers in the health system
Dr Nixon Niyonzima, the head of research and training at UCI, says the lack of access to diagnostic facilities, cost of diagnostic services, and distance to health care facilities are some of the barriers in the health system.
“There are screening services at every health centre II, III and IV and regional referral hospitals. A self-breast examination can be done at home while a trained health worker can perform the clinical breast exam. If there is a lump, an ultrasound scan or mammography can be done to analyse the mass, followed by biopsy where indicated,” he says.
While the ultrasound scan is present in almost every corner of Uganda, health workers need adequate training to interpret the images. Mammography, which is more precise, is only present in a few hospitals – mostly in Kampala.
“Cancer is not a death sentence but patients present late, which makes the treatment outcomes poor. The government is providing funding for provision of cancer care services through the UCI. It is also setting up regional cancer centres in Gulu, Arua, Mbale and Mbarara districts, to improve access to treatment,” Dr Niyonzima adds.
Social challenges
Women suffering breast cancer endure a profound array of difficulties that extend beyond the medical realm, deeply affecting their domestic lives and body image.
The stigma surrounding the disease means some may experience a shift in their relationships with partners and family members, leading to feelings of isolation, withdrawal of emotional or physical support. This strains the bonds of intimacy in any relationship.
Some rural women, who do not have resources, need financial support from their husbands to access treatment. The husbands, as a result of stigma, may choose to marry other ‘healthier’ women, abandoning their sick wives to fate.
“Women usually seek medical attention without their husband’s support and if there are decisions that are made, many husbands do not understand them. They become indifferent to their wives after they have lost their breasts,”Atwine says.
In the urban setting, women, who are primary caregivers in the home, have to balance work and treatment. The prohibitive cost of treatment leads to financial stain, which in turn increases the level of stress in the household.
The inability to perform daily chores or care for children can lead to feelings of guilt and inadequacy, impacting their mental health. Women may find themselves without access to necessary resources, counseling, or community support, leaving them to navigate their journey alone.
“Cancer treatment does not leave you the same. It affects the people around you, especially the children. Their mental health is strained because they live in fear that you will die. Sometimes, the children stop going to school,” Akello says.
Delays in seeking medical care reduce survival chances of the patient. This in turn, causes a need for aggressive treatment, which makes patients susceptible to late effects.
“These effects can come months or even years after treatment ends, and they include infertility, progressive organ damage, heart disease, diabetes and secondary cancers which are life threatening. For the first three years after cancer treatment, patients are under surveillance to catch any relapses,” Dr Niyonzima says.
After three years, the risk of a relapse is very low so the focus turns to looking out long effects the patient may have suffered. The fact that cancer therapy is very long remains an unsolved challenge
“We may be survivors but every day, we are at the risk of a recurrence. This fear makes us feel imprisoned. There is a need for counseling and rehabilitation to help us cope with the life after the treatment and love and support from people around us. We need empowerment to attain financial stability,” Akello appeals.
A ray of hope
Hilda Mwesigwa received a breast cancer diagnosis in July 2011 and completed her treatment in February 2012. She has been cancer free for 13 years.
She is a board member of Uganda Women Cancer Support Organisation (UWOCASO) and a member of the Malaika Angels Group, that counsels cancer survivors and caretakers.
“I share my breast cancer story because there is a lot of stigma. This gives hope to those undergoing treatment that they too can fight and win the battle. I owe the strong will I had to fight cancer in 2011 to a breast cancer survivor who talked to me and gave me hope,” she says.
Mwesigwa participates in breast cancer awareness events such as golf-tournaments and dance workouts, to create awareness.
“I implore women to go for screening during this breast cancer awareness month of October. Spouses of breast cancer patients should love and support their partners during treatment. Husbands might be tempted to look elsewhere for love and care but this can quicken the death of their wives,” she adds.
The government is increasingly recognising the need for comprehensive cancer care. Recent initiatives aim to improve screening programs, enhance public health education, and secure funding for cancer treatment.
These efforts are critical in shifting the narrative around breast cancer from fear and stigma to empowerment and hope. As Akello reflects on her six-year journey on cancer treatment, she emphasises the importance of awareness.
“If I had known more about what to look for during self-examination, I would have acted sooner. I had the lump in my breast for about three years yet I did not care to find out what it was. I believe that education can save lives. This is why I want to share my story with others and give them hope that even with a stage IV diagnosis, you can live,” she says.
Various organisations including UWOCASO, Rays of Hope Jinja, Uganda Cancer Society and others have made strides in raising awareness.
“I now volunteer with UWOCASO. We empower each other and share stories. It makes a difference because we find strength in shared experiences, encouraging one another to stay resilient through treatment,” Akello adds.
Despite increased awareness, Uganda’s healthcare system struggles with limited resources and many hospitals lack adequate facilities for cancer diagnosis and treatment.
Community health worker programs have been introduced to bridge this gap, providing information and referrals to women in remote areas. However, transportation costs and cultural barriers still pose significant obstacles.