Prime
Government issues new Ebola dos and don’ts

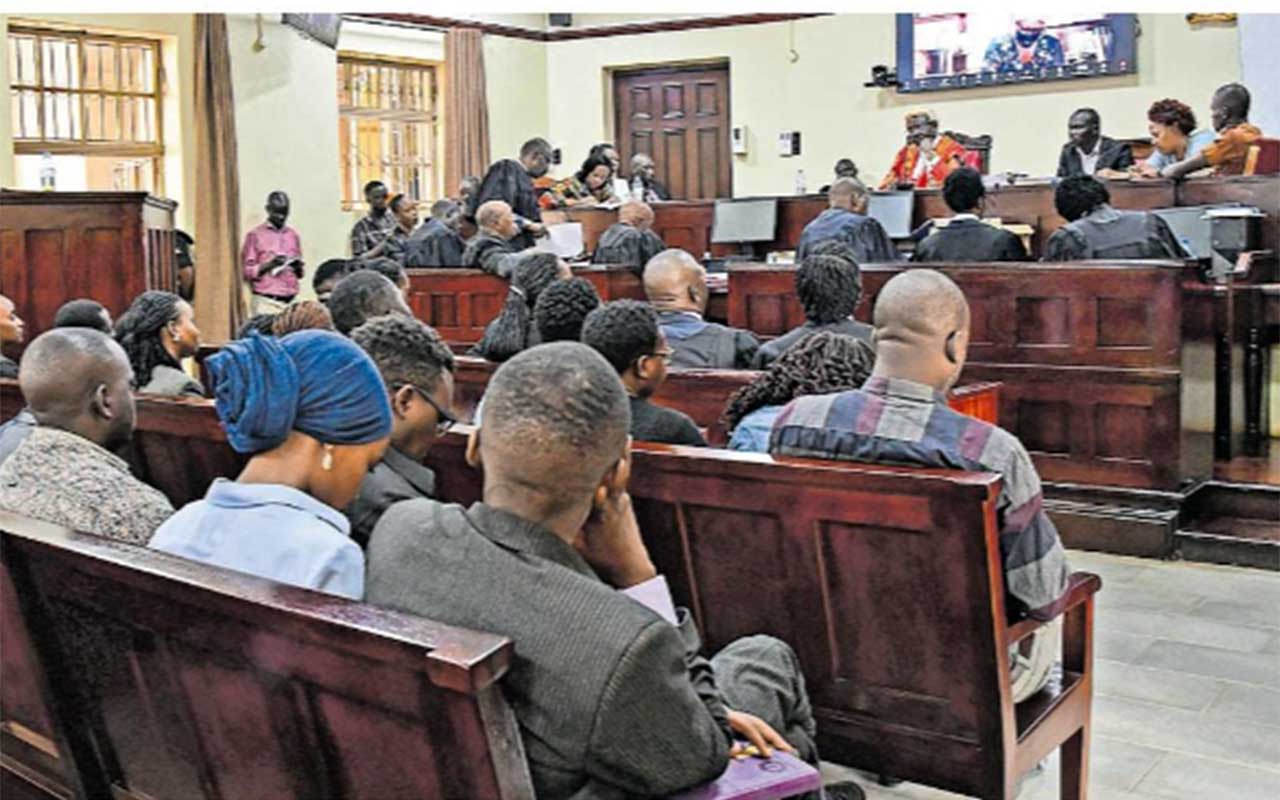
Health workers in Mubende District prepare to transport the body of an Ebola victim for burial on September 20, 2022. PHOTO/BARBRA NALWEYISO
What you need to know:
- The new SOPs cover hand hygiene and personal protection, injections and management of sharp objects, among others.
The Ministry of Health yesterday issued a raft of new measures and standard operating procedures (SOPs) to inform national response to the contagion- and stem its spread.
The SOPs target mainly health workers, communities, and family members, among other stakeholders that find themselves at the frontline in fighting a virulent disease that kills 40-90 percent of victims.
The release of the guidelines by the Health ministry and World Health Organisation (WHO) followed the confirmation, on Tuesday, by the government of an outbreak of Ebola Sudan in the country.
This newspaper was the first to break the story.
The disease, Health ministry said, had killed one person, a 24-year-old man, from Ngabano Village in Madudu Sub-county, but there was no certainty how he contracted the disease.
There had been six prior suspect deaths that residents and health workers attributed to an inconclusive disease, and five of the dead were from the same family, according to our findings.
Ebola is transmitted from person-to-person through contact with the body fluids or blood of an infected person and takes between two days to three weeks to manifest, according to WHO.
Following news of the outbreak, supervisors placed frontline health workers on the highest level of alert, suspicion and vigilance in dealing with patients who present with symptoms similar to that of Ebola.
These include high fever, vomiting, bleeding from body orifices, sore throat and mouth as well as fatigue and severe pains.
According to the Ministry of Health, there are higher survival chances if treatment is commenced early. Experts advise that caregivers should provide plenty of drinks – water, soup, tea or locally available beverages - to an Ebola patient and, if possible, encourage them to feed “little by little, spoon by spoon
The new SOPs issued yesterday cover hand hygiene and personal protection, injections and management of sharp objects, laboratory sample management, and autopsies and burial management and reducing the risk of home infections.
SOPS TO FIGHT EBOLA
Hand hygiene and PPEs
• All health workers, including aides and cleaners, as well as visitors to use personal protective equipment (PPE) and wash or sanitise hands regularly.
• Scrub or medical suits, not personal clothing, to be worn in patient care areas.
• Do not touch eye, nose, or mouth after contact with used gloves and gowns.
• Do not re-use disposable PPE.
• Thoroughly clean and decontaminate reusable equipment.
• All waste generated during decontamination should be treated as infectious waste.
Injection safety and management of sharps
• Limit use of needles and other sharp objects and never reuse injection or parenteral medical equipment on another patient.
• Never replace the cap on a used needle or direct the point of a used needle towards any body part.
• Dispose of syringes, needles, scalpel blades and other sharp objects in puncture-resistant containers.
Cleaning and waste management
• Cleaners should wear rubber gloves, impermeable gown and boots and facial protection while at work.
• Regularly clean and decontaminate surfaces, including floors.
• Soiled linen should be placed in clearly labelled, leak-proof bags or buckets at the site of use.
• For low-temperature laundering, wash linen with detergent and water, rinse and then soak in 0.05 percent chlorine for approximately 30 minutes.
• Waste should be segregated at point of generation to enable appropriate and safe handling.
• All solid, non-sharp, infectious waste should be collected in leak-proof waste bags and covered bins.
Safety with laboratory samples
• Limit use of phlebotomy and laboratory testing to essential diagnostic evaluation and patient care.
• Follow World Health Organisation (WHO) recommendations for procedures to safely collect blood or other samples from persons suspected or confirmed to be infected.
• Laboratory personnel handling potential Ebola Virus Disease (EVD) clinical specimens should wear full PPE, particulate respirators or powered air purifying respirators (PAPR).
• All laboratory sample processing should take place under a safety cabinet, or at least a fume cabinet, with exhaust ventilation.
Post-mortem examinations
• Post-mortem examination should be limited to essential evaluations and performed by trained personnel.
• Personnel should use PPE including eye protection, mask (a particulate respirator or a PAPR if performing internal autopsy), double gloves and disposable impermeable gowns.
• Specimens should be placed in clearly-labelled, non-breakable, leak-proof containers and delivered directly to designated specimen handling areas.
• All external surfaces of specimen containers should be thoroughly disinfected prior to transport.
Managing exposure to virus
• Stop current task or patient care and safely remove PPEs upon exposure to blood, body fluids, secretions, or excretions of confirmed or suspected Ebola patient.
• Leave patient care area, wash affected skin surfaces with water and soap.
• Promptly report incident to the local coordinator.
• Exposed persons should be medically evaluated, including fever monitoring twice a day for 21 days.
Burial protocol
• Wear mask, eye protection and double gloves or heavy duty gloves and rubber boots or closed puncture or fluid-resistant shoes and overshoes to handle the dead body of person who has died of suspected or confirmed Ebola.
• Do not spray, wash or embalm the dead body.
• Place the body in a double bag, wipe over the surface of each body bag with a disinfectant (e.g., 0.5 percent chlorine solution) and seal and label with the indication of highly infectious material.
• Remove PPE immediately after the procedure and wash or sanitise hand after removing PPE removal.
• After wrapping in sealed, leak-proof material bag, the dead body should be immediately moved to a mortuary and placed inside a coffin, if possible, and buried promptly.
Reducing home transmission risk
• Individuals at risk include those that spent time with, attended burial of an Ebola victim.
• Provide Ebola patient own space, separate from the rest of the family.
• Use separate plate, cup, and utensils (spoon, fork), toothbrush, and other items
• Designate one family or community member to care for Ebola patient.
• Avoid physical contact and treat all of an Ebola patient’s body fluids including stool, vomit, blood, breast milk, sperm, urine and sweat as dangerous.
• Wear impervious gloves if carer must touch patient, and put soiled clothes, towels and bed linens in a plastic bag and incinerate.
• Use PPEs if providing extended care at home to Ebola patient, and regularly wash or sanitise hands.
• If the patient vomits, has diarrhoea or starts to bleed, transported them immediately to a hospital.
Source: Health ministry