How endless doctors’ strikes have crippled health facilities

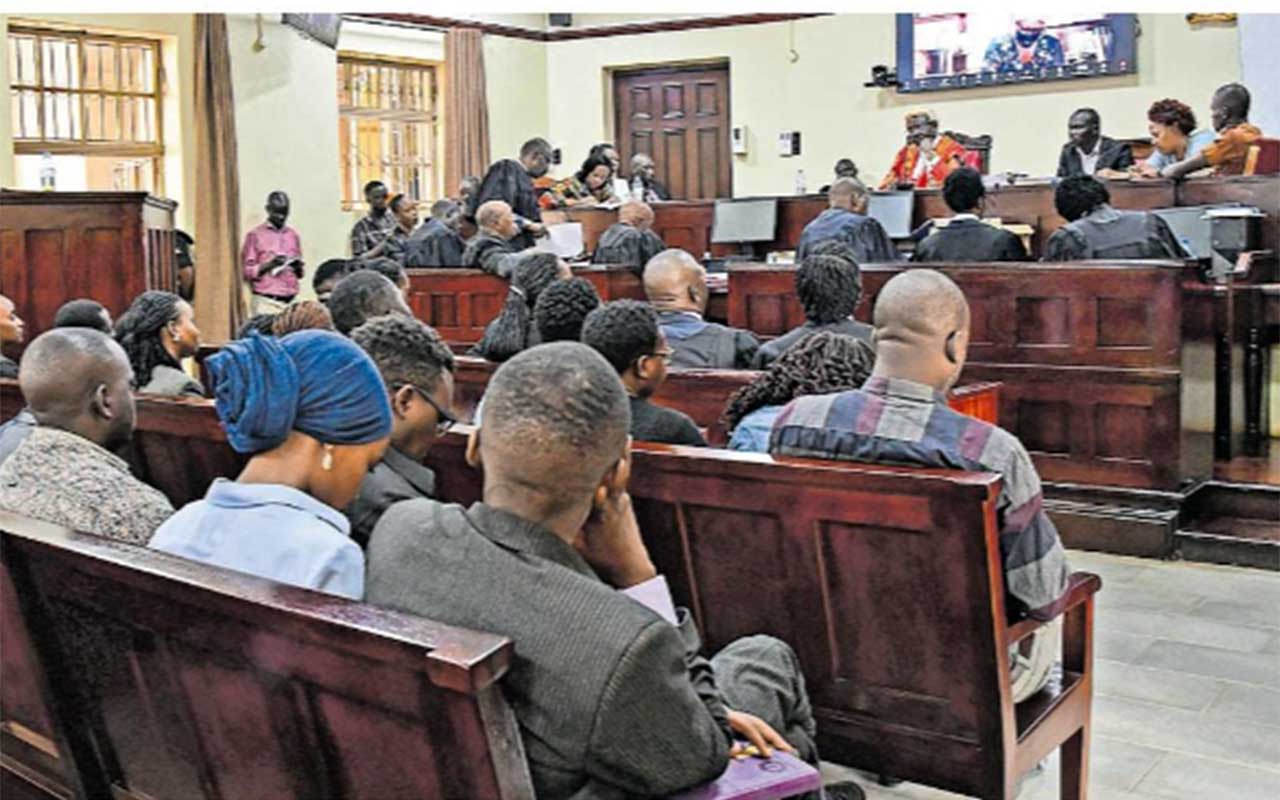
Ugandans seek medical services at Wellness Clinic in Mulago Hospital, Kampala, last week. PHOTO/JANE NAFULA
What you need to know:
The government has appealed to medical specialists and Senior House Officers to prioritise patients, saying the pay grievances are being worked upon
The crack of yesterday’s dawn found Mr Brian Mukasa, a resident of Makindye Division in Kampala City, at the corridors of Mulago National Referral Hospital surgical unit.
Mr Mukasa, and other patients, who needed specialised services, were still waiting to see a doctor at 1:30 pm. The hard benches placed on the cold corridors of the unit were still fully occupied. The unit is for outpatients.
“I arrived here very early in the morning. But up to now, I haven’t seen a doctor,” Mr Mukasa said.
“They have registered my name and I hope I will be handled,” added.
The situation was not any different from what our reporters observed at Kawempe Hospital. Ms Nancy Nalubwama, a resident of Old Kampala, said she arrived at the facility at around 7 am. She was yet to be handled at around 11 am.
A caretaker of another patient at Kawempe Hospital, Ms Lydia Katusiime, said her sister was delivered normally last night at the hospital. However, she told our reporter that by 11 am, no doctor had come to check on them since Monday night.
Dr Irene Asaba, a surgeon at Mulago Hospital, said specialised facilities such as Mulago and Kawempe hospitals have very few specialists to handle patients speedily.
Dr Asaba said they were operating more efficiently when Senior House Officers (SHOs) hadn’t gone on strike and medical interns were around.
SHOs are qualified doctors who are training to become specialists. They said they went on strike on May 1 due to the government’s failure to pay them for the last four to six months they have worked.
“We had been bearing the burden with SHOs, but now that they are not there, we are saying enough is enough,” Dr Asaba, a Medical Officer Special Grade (MOSG) alias specialist doctor, said.
“We are doing, even more, this season. This is because of the complementary workforce such as SHOs and interns who are either working partially or are not deployed,” the surgeon added.
The SHOs and interns, according to Uganda Medical Association (UMA), carry around 60 percent of the workload in public facilities because of the few doctors employed by the government. Interns have also been waiting for deployment for the last nine months, UMA said. Interns are qualified doctors who are on hospital placement to get permanent practising licenses.
Leaders of the MOSGs, during a press conference organised by UMA in Kampala yesterday, also threatened to go on strike effective. They said the government has failed to address the discrepancy in salary structure for doctors which they have been raising for over a year.
The MOSG said the Shs6m difference between their pay and that of consultants is too much to swallow because they have the same qualifications and the only difference is years of experience. They want the government to increase their pay from Shs6 million to Shs11m. Consultants currently earn Shs12 million.
“Emergency services by SHOs and associate consultants (MOSGS) have been withdrawn,” Dr Joel Kimera, a paediatrician and the leader of MOSGs, said yesterday.
Dr Kimera, however, said their immediate supervisors, the consultants and senior consultants will provide the emergency services.
“The only issue is that they [consultants and senior consultants] are few – around 250,” he said. “Medical officers will also continue working, so Ugandans can come and get emergency services. But the three carders of interns, SHOs and associate consultants will not be there,” Dr Kimera warned.
However, the Health ministry spokesperson, Mr Emmanuel Ainebyoona, appealed to the specialists and SHOs to prioritise patients, saying the government is handling their issues.
“They [striking doctors] need to be patient because the government is resolving various complaints they have raised,” he said, adding that the issues will be handled at the Cabinet level.
Both Dr Kimera and Dr Herbert Luswata, the secretary general of UMA, when asked about their priority and the fate of the patients, said the strike is meant to improve the quality of services in the long run.
Dr Diana Atwine, the Permanent Secretary of the Health ministry, has, however, maintained that the SHOs should continue working as the government looks for money to pay them and also deploy medical interns.
Dr Chris Baryomunsi, the Information minister, said doctors should concentrate on work because the government is going to handle their issues.
“We appreciate the work SHOs and interns do, money will be found to clear the arrears, it’s the government’s position,” Dr Baryomunsi said while applauding to SHOs who are providing emergency services.
The minister also said there are concerns about the capacity to continue paying the SHOs and interns.
“Right now, their questions around the quality of training and the ability of the government to afford to pay [allowances or salaries] for interns. These are issues that should be discussed to avoid the disruptions [in access to care] caused by the strikes,” he said.
However, Dr Herbert Luswata, the secretary general of UMA, while announcing the strike by MOSG, said the government has not been forthcoming about resolving issues raised by aggrieved doctors.
He said each intern doctor and SHO, according to the directive from the President, are supposed to be paid an allowance of Shs2.5 million per month.
Dr Luswata said this money is for their welfare as they bridge the gap in service delivery which has resulted from the low number of doctors employed by the government.
“The specialists have been trying to cover this gap created by SHOs who are on strike. But the challenge we have is that the specialists who have been covering this gap are also starting their strike tonight (Tuesday night),” Dr Luswata said.
He warned that the strike would increase deaths in hospitals.
“The situation is going to become worse. We are likely to see more people coming to the hospital and staying the whole day without anyone attending to them. But we hope those who are remaining will take care of patients so that deaths do not increase,” Dr Luswata said.
Treatment standards
The current rate of 1 doctor to 20,000 people is below the World Health Organisation standard of 1 doctor to 1,000 people.