Uganda met with shortage of 180,000 health workers

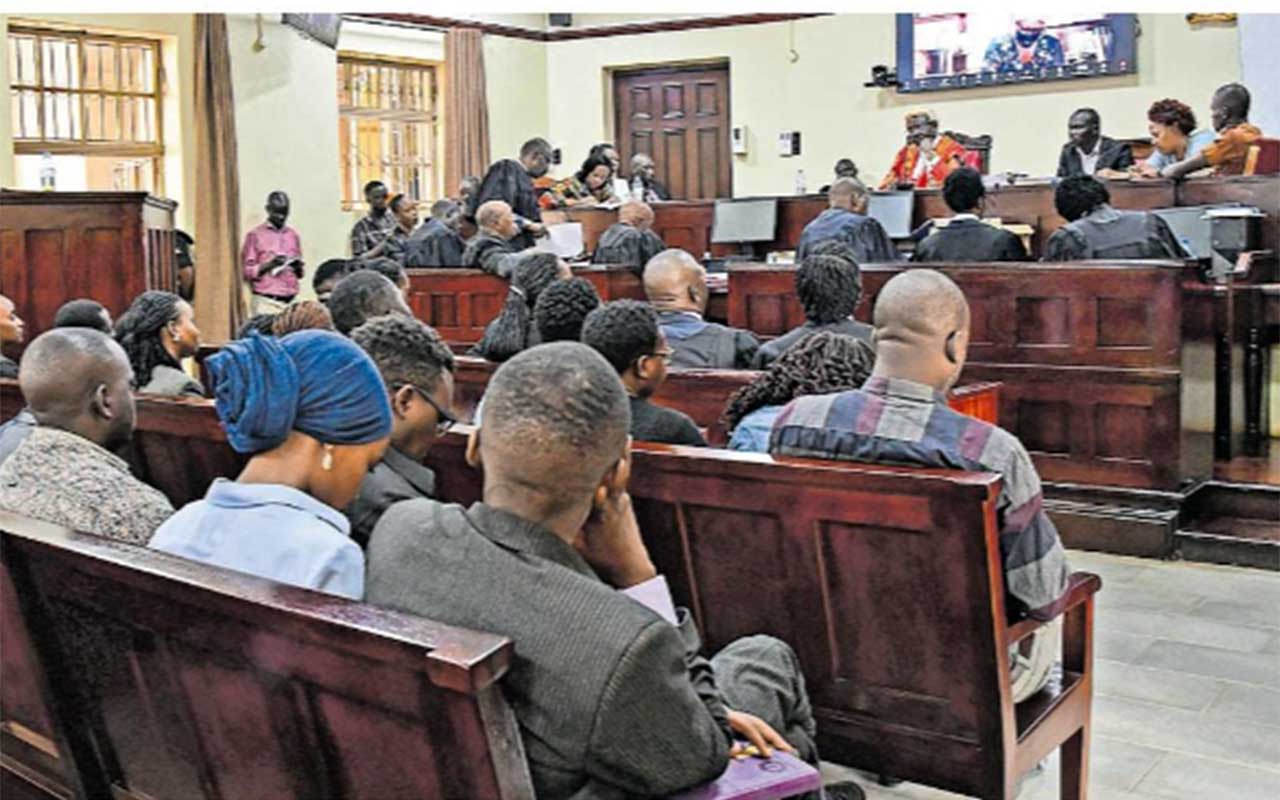
Dr Yonas Tegegn Woldemariam, the World Health Organisation Country Representative to Uganda (right) and Prof Pius Okong, the chairperson of the health service commission in Uganda, append their signatures on the dummy of an analysis of the health labour market report launched during the national policy dialogue on the health workforce in Uganda in Kampala on June 27 as Dr Charles Olaro (left) from the Ministry of Health looks on. Photo/Jane Nafula
What you need to know:
Health experts express concern that Uganda’s chronic understaffing in the health sector denies citizens access to quality and timely healthcare services
Donors and health experts have expressed concern over the chronic understaffing in the Ugandan health sector, a challenge that they claim continues to deny Ugandans access to quality and timely healthcare services.
Dr Alfred Draweli, the commissioner for institutional capacity building and human resource development in the Health ministry, revealed that it is currently grappling with a workforce shortage of more than 187,000 health professionals.
“…given the types of diseases we are dealing with, and the standards we have set, Uganda requires a workforce of about 342,832 cadres as opposed to the current 155,000 cadres,” Dr Draweli revealed during the national policy dialogue on the health workforce in Uganda organised by the World Health Organisation (WHO).
He added: “This is a huge gap because it is just half of what we need.”
During the dialogue, the analysis of the health labour market was launched. The report indicated that currently, there are 7,793 medical doctors and specialists in Uganda, of which 25 percent are employed in the public sector and 39 percent in the private sector. The report also revealed that the nursing professionals, both in the public and private sector are 73,956; midwifery professionals (32,959); dental surgeons (504) while the population of pharmacists stands at 1,712.
Dr Jane Ruth Aceng, the Health minister, said training, recruiting and retaining of human resources for health, is an emergency that the ministries of Finance and that of Public Service must embrace. This can only be done, Minister Aceng opined, by ensuring timely release of wages and recruitment of the required health workers respectively.
“When you want to recruit, you need clearance from Public Service [ministry], which may take eight months, and when you delay to recruit, the permanent secretary gets a letter asking her to return the money, you request for the theatre cadres, but you are only given an anaesthetic officer without a theatre nurse. Do these people understand that some of the health cadres work as a team?” the visibly disappointed minister wondered.
Minister Aceng further noted that it is common knowledge that the health sector cannot progress and achieve Universal Health Coverage (UHC) without a formidable workforce needed to increase access to essential services.
“About 1,500 health professionals are churned out of training institutions annually and very few are recruited into the system and hence the challenge continues,” the Health minister said.
Ms Margaret Babiwenda, the principal human resource officer in the Department of Human Resource and Planning, Ministry of Public Service, said: “The health sector should understand that no recruitment can happen without a sufficient wage. All the concerned ministries must come to a round table and address the issue at hand, otherwise, the Ministry of Health will continue to blame us.”
On the issue of the bureaucratic nature of clearing the Health ministry to recruit staff, Ms Babiwenda said this was no longer an issue. Clearances, she clarified, are now done instantly.
Prof Pius Okong, the chairperson of the Health Service Commission, revealed that the Education ministry is currently grappling with a deficit of Shs176 billion needed to bridge the existing staff gap in the 17 regional referral hospitals. He noted that there are currently 270 emergencies at regional referral hospitals requiring surgery, but some of these cases might be attended to by interns due to scarcity of specialists.
“There are about 270 emergencies requiring operations at regional referral hospitals. But who is managing the patients? They are interns,” he exclaimed.
Prof Okong also disclosed that a third of maternal deaths recorded in these hospitals occur among mothers who are not attended to by specialists. He also asked the Ministry of Public Service to consider lifting the staffing ceiling that puts a cap on the number of health workers that must be recruited.
WHAT THEY SAY...
Dr Yonas Tegegn Woldemariam, the World Health Organisation country representative to Uganda, said multi-sectoral collaboration and commitment are needed to mobilise resources and have “one plan, one budget and one agreement to invest in the health sector and improve the wellbeing of the populace.”
Dr Flavia Mpanga Kaggwa, a health specialist at Unicef Uganda, challenged Uganda to scrutinise the quality of health workers trained by the private sector.
Dr Diana Atwine, the Permanent Secretary of Ministry of Health, called for a regulatory framework that will check the exploitation of health workers, who leave the country in search of greener pastures.
Dr Charles Olaro, who represented the Director General of Health Services, Dr Henry Mwebesa, said while the government had invested in the infrastructure and equipment, the returns would be minimal without investing in the health workforce and optimally utilising the available workforce.
Prof Francis Omaswa, the executive director of the African Centre for Global Health and Social Transformation, said they need governments to establish the recruitment code for migrant health workers to ensure they are paid well and allowed to develop professionally.