Prime
Remembering the wave that blindsided us

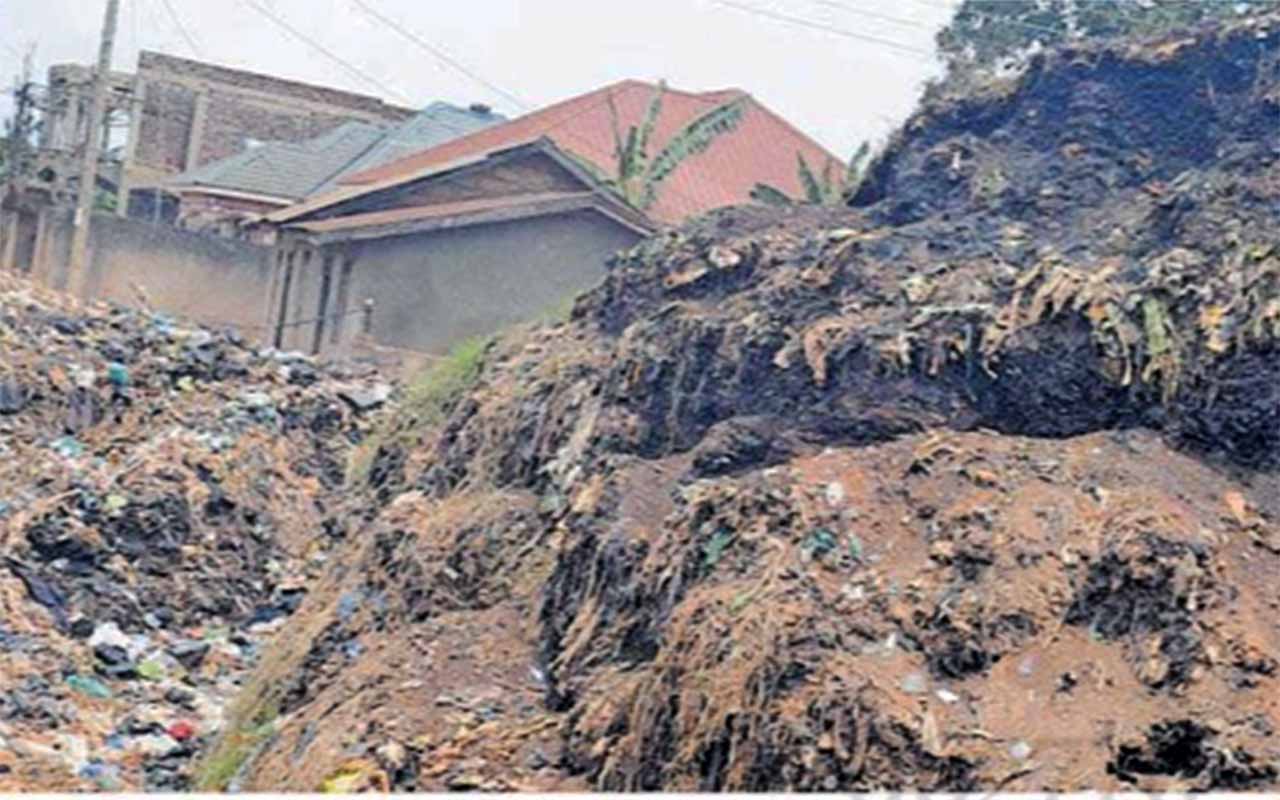
Health officials from Entebbe Hospital bury a Covid-19 victim last year. At one time, the hospital registered between five and eight deaths daily. PHOTO / FILE
What you need to know:
- Many found it odd that their president was the only one to sport a shield of protection at the event in the Rwandan capital of Kigali.
- Mr Museveni has worked tirelessly and obsessively to contest narratives that speak of Covid-19 as a run-of-the-mill pathogen.
President Museveni’s decision to mask up during the official opening of the 2022 Commonwealth Heads of Government Meeting (Chogm) at the backend of June was viewed with condescension, even contempt, by Ugandans.
Many found it odd that their president was the only one to sport a shield of protection at the event in the Rwandan capital of Kigali.
Mr Museveni has worked tirelessly and obsessively to contest narratives that speak of Covid-19 as a run-of-the-mill pathogen.
His leadership has adequately conveyed that the pandemic has not gone away. On July 20, he used a national address to reveal a close shave with Covid-19 while in Kigali on Chogm duties.
“When we went for a smaller meeting, I relaxed a bit and I removed the mask and I was sitting with Boris Johnson, the Prime Minister of Britain, and a man from Tuvalu, a small island with 12,000 people, and the man had Corona. I sat with him for almost one and a half hours,” he said.
He added: “So when I came back and I went to Ntungamo… I self-isolated myself and they did rapid tests then. I quarantined myself… and I had no problem. So this could be because of this vaccination. Definitely, I was sitting near this man and he even spoke. He didn’t cough, but he spoke as part of the contribution…”
If Mr Museveni wanted to tell Ugandans that a victory lap had been taken prematurely, he emphatically did so.
He also used his national address to remind the country of its sluggish vaccine rollout, with 4.6 million adult Ugandans still unvaccinated.
On an encouraging—if no less heart-warming—note, he revealed that a potential fourth Covid-19 wave had been averted.
Since registering its Covid-19 index case on March 22, 2020, Uganda’s Covid-19 tale has had various moments, some good, none great, some terrible.
The epidemio-logical picture of the Covid-19 variants that sent Uganda into some kind of existential panic forecasted a challenge that would prove enduringly difficult to suppress.
After Alpha triggered a global spike in cases, Beta made young people sicker. Not to be left out, Gamma reinfected those who had already recovered from the flu. All three strains registered on Uganda’s radar, but it was Delta that blindsided the country’s healthcare system.
The doomsday variant was responsible for a second wave of infections that was replete with hospitalisations and deaths. The wailing of ambulances cut into the soul of Uganda’s major cities as the wave that started in late May of 2021, left overburdened facilities short on oxygen cylinders.
By the time the wave started to plateau out at the backend of July—nearly a year ago—Delta’s infectiousness had made Uganda’s route out of the pandemic that much more complicated.
Entebbe Regional Referral Hospital—where the country’s patient zero beat off the pathogen way before electioneering activities triggered the first wave of infections in December of 2020—at first glance looks unremarked.
As the second wave left health officials more worried than they cared to admit, medical practitioners at the 200-bed facility found themselves waging a brutal battle for victory.
Dr Andrew Menya used to split his working hours between Entebbe Regional Referral Hospital and Mukono Church of Uganda Hospital.
He remembers Delta displaying a level of transmissibility that only added to a sense of confusion and exhaustion for the medical practitioners.
“We had to be confined in the hospital for close to five months,” he said of the height of the second wave that kept him rooted in Entebbe.
As Uganda experienced an explosion of Covid-19 infections, Delta’s enhanced ability to prey on the vulnerable was not lost on many.
Dr Menya, who takes care of his elderly parents, had to rule out any visits. Inside the proverbial four walls of Entebbe Regional Referral Hospital, doctors on the frontline were breaking down.
The doctors were scarred after speaking with dying patients they were unable to treat because of a dearth of beds.
“I worked day and night trying to save lives, but sometimes in vain,” Dr Menya recalled. “What haunted me most was to see people die while calling my name.”
With Entebbe Regional Referral Hospital sinking beneath the weight of Delta infections, Dr Menya also found himself doing something he was not taught at medical school. “We were forced to carry oxygen cylinders from the store to the wards.” Hospitals are sensitive to the rate at which viral waves grow and peak: slow is better, fast is worse. The second wave made the oxygen cylinders that Dr Menya and his colleagues wheeled into wards a modicum.
Such was the surge in cases that with oxygen running out and hospital beds full, patients continued to pour in with oxygen tanks in their cars. Still, Dr Menya would count anywhere between five and eight deaths each day.
“One would wait for another to pass on or get discharged to get space and be attended to,” Dr Menya told Sunday Monitor, admitting, “It was challenging.”
Zero-Covid approach
This was a far cry from the period preceding the first wave of infections when Uganda went for a zero-Covid approach. In July of 2020, Dr Menya was part of a feel-good story after he delivered a baby to a mother stricken with Covid. The story was headline news, taking different TV crews to Entebbe Regional Referral Hospital.
“I was chosen with my fellow medical officer, Dr Emma Lwamutwe, to take lead,” he recalled, adding, “I got a call from my superior at night that she was to give birth but could not push the baby. A caesarian section was to be undertaken.” It was a resounding success.
“God was on our side. We prepared well with a team of nine other people, including nurses. Each one of us knew what to do at the time,” he said. “We delivered her well with a baby girl, and none of us was infected.”
A year later, in early July 2021, the gains of Uganda’s zero-Covid approach had been steadily eroded. It didn’t help matters that Covid jabs were not finding arms. Positive cases from the Delta variant averaged between 10 and 15 at the hospital.
Yet several months after hospitalisations and infections plateaued out, the government did the unthinkable. Dr Menya and other medical practitioners, who were enlisted to rein in Covid, were cut loose.
Dr Menya has not given into the outpouring of bitterness at his circumstances. He told Sunday Monitor that he prides himself in the rigour of the work that he did and “my dedication towards serving the country.”
The manner in which Dr Menya and others were cut loose raises questions around whether Uganda learnt the right lessons from the pain inflicted by the doomsday variant.
The question around Uganda’s moribund health infrastructure particularly remains outstanding. On July 12, stakeholders in the health sector were keen to show that lessons have been learned.
Seventy emergency responders were commissioned after undertaking a fortnight-long training under the auspices of World Health Organisation’s (WHO) Rapid Response Teams Training Implementation Package (RRT TIP).
“The establishment of trained Rapid Response Teams, readily available for deployment and response in emergencies, is critical in addressing the country’s public health and emergency problems,” the Health minister, Dr Jane Ruth Aceng, said.
Dr Yonas Tegegn Woldemariam, the WHO representative to Uganda, added: “Covid-19 has highlighted the need for skills transfer at the national and sub-national levels. The trained national trainers will be able to conduct and use their knowledge to build the capacity of Rapid Response Teams at the national and subnational levels to effectively and efficiently respond to public health emergencies.”
Dr Amy Boore from the US Centers for Disease Control and Prevention Uganda, said: “Building capacity for multidisciplinary teams at all levels is critical for immediate effective and efficient response to avoid devastating impacts.”
Mr Robert Ngudo, a resident of Kitoro in Entebbe, knows firsthand what devastating impacts feel like.
He lost his brother and mother in a space of a week during Uganda’s Covid reckoning last June. His brother, Charles Ngudo, died as they tried to put together Shs4.5m to buy an oxygen cylinder.
“His last words were, ‘brother, I need to breathe. Get me something.’ That was on June 12,” Mr Robert Ngudo poignantly recalls.
“After burial in Jinja on June 18, we got information that our mother had contracted Covid and was in isolation. Shortly after, she was pronounced dead. What pains me is I did not even have a chance to say my goodbyes.”
Many households across the country share his pain and would give anything for lightning not to strike twice.