Prime
Tororo hospital on the spot over maternal deaths

An attendant rolls a patient to the theatre at Tororo General Hospital. Delays in receiving adequate treatment at health facilities increase the risk of maternal deaths. Photo | File
What you need to know:
- Relatives of former patients at the facility say they lost loved due to the negligence of health workers and corruption.
Dominic Ochieng, a resident of Akadot sub-county in Tororo District, is still grappling with the loss of his wife and an unborn child.
Elizabeth Aswan died on February 23 at Tororo General Hospital where she had been taken to give birth.
When the Monitor visited the family home, grief hang heavy over the kempt homestead. The home consists of a modest shamba that is well-tended and dotted with fruit trees and pine that provides ample shade. A fresh floral wreath lies on Aswan’s grave in its humble setting, holding the lasting vestiges of her living years.
A downcast Ochieng attempts to put up a brave face as he recounts the events of that fateful day.
“My wife was in labour and I took her to Tororo hospital where she was admitted. After a while, a nurse asked me for some money but I told them I didn’t have any at [that] moment. The nurse told me to do whatever I can to get some money. I decided to leave the hospital to look for the money. I left my mother and sister attending to my wife. At home, I sold whatever I had and got some money,” he says.
He adds: “Unfortunately when I returned to the hospital, I found my mother and sister crying. I asked what the problem was and they told me the nurse had informed them that my wife and child may not survive. So, they proposed that they give her a blood transfusion. I went to speak to the nurse but was informed that my wife had died. I went and checked for myself and indeed my wife and child had died.”
The body was then taken to the mortuary where Ochieng was asked to pay Shs40,000 to have it treated.
Patients have a right to impartial access to medical care in government health facilities. In the event of a medical emergency, under the Hippocratic Oath, a person is entitled to receive emergency medical care unconditionally without having to pay any deposits or fees prior to medical care.
The principles of the Hippocratic Oath are held sacred by doctors to this day.
“Treat the sick to the best of one’s ability, preserve patient privacy and teach the secrets of medicine to the next generation,” the oath reads in part.
Ochieng’s account suggests that his wife was denied the right to health care at Tororo hospital and the consequences were fatal.
“I came home to arrange transport for the bodies. The police helped to transport the body to Mbale for the post-mortem and we returned home where she was buried. After the burial, we opened a case against the nurses and took the post-mortem report to the police who promised to call us. Up to now, I have never received a call from the police. It is my appeal to the government that I am availed justice,” he says.
The maternal mortality ratio for women aged 15 to 49 in Uganda is 368 deaths per 100,000 live births compared to 438 deaths per 100,000 live births in 2011, against a target of 70 deaths.
This significant decline notwithstanding, severe bleeding accounts for one in four maternal deaths globally and in Uganda bleeding accounts for 46 percent of maternal deaths. There is evidence that the skill and diligence of health providers is decisive in preventing the loss of life.
As such, Ochieng’s ordeal brings the competencies of the health staff at Tororo Main Hospital into sharp focus. The post-mortem findings added credence to Ochieng’s account, according to Joram Okook, a relative to the deceased and a councillor representing Morokatipe Sub-county claims.
“When they realised the situation had worsened, they tried to rush her to the theatre but unfortunately, she did not make it. Both the mother and the unborn baby boy. I learnt of the girl’s demise and the two bodies were picked and taken to where the girl was married somewhere in Akadot,” Okook says.
He adds: “I went there on February 24 on the day of the burial and when I learnt of how the incident happened, I said this is criminal. It is when I called the RDC Mr. Nixon Owole. I recorded a statement with Police. So, we demanded for a post-mortem to be carried out.”
He further says: “I objected to the post-mortem being carried out in Tororo Main Hospital since that is the very place where the incident happened. I demanded that the post-mortem be done in Mbale and the Police cooperated.”
Perhaps without Okook’s intervention, the post-mortem may not have been carried out.
Maternal deaths are common in the 200-bed ailing government facility in Tororo. The health facility serves a catchment area of 500,000 people extending to the Kenya-Uganda border and beyond. The six-bed labour suite is staffed with two to three birth attendants supervised by one to two physicians who can barely manage to attend to the scores seeking their services.
The birth attendants collect patient information by filling out handwritten birth registers on admission and discharge. It is these hospital records that informed Okook’s sense of injustice.
“The post-mortem report came out and it was pinning the hospital for negligence. I am dragging the hospital to court so we shall leave no stone unturned in search for justice. We can’t also rule out the possibility of bribes. At one time they were arrested then they were granted bail. There were three nurses and a doctor. It was actually the people on duty that day,” he says.
Francis Odoi, a nurse at Osukuru Health Center III, took his wife Christine Maliza Mukisa, a 34-year-old mother of four, to the hospital when she started experiencing labour pains. However, she later passed away. Odoi says the sight of her grave still causes him pain.
The sense of loss is palpable as he narrates the events of the fateful day.
“I escorted my wife to Tororo hospital and we arrived at about 8:30am. I went to the labour suite and found a doctor, midwives and two other mothers. When they finally called my wife, they said she was not yet [ready to give birth]. My wife later went back to the health workers and was told her that she would [be ready to give birth] at 2pm. However, when she ended up giving birth outside the labour suite at 9.45am,” he says.
He adds: “People gathered and that is when the midwives rushed her inside the labour suite. The baby was put on oxygen. At 2pm, my wife started bleeding seriously. I tried to enter the suite but was chased away by the health workers. They said she was bleeding so much and that they wanted to transfer her to Mbale Regional Referral Hospital. I was told to go and buy a drug to stop the bleeding. I rushed to town to get the drug.”
He further says: On my way back, they called me and said I was delaying and they were going to remove her uterus. They told me to hurry and sign [the documents approving the surgery]. When I finally got to the hospital, I was told that an ambulance is on its way to pick us up and take us to Mbale. I waited until 5pm but no ambulance came. They then told me that blood had been brought from Nagongera and they were going to try and help her but added that they were not sure she would make it. At 6pm they told me she has passed away.”
Moses Mugwe, the spokesperson of Bukedea South Region, told the Monitor that Mukisa’s death was a result of rash and negligent behaviour by the health workers.
“That matter was reported here and it was investigated in February 2023 and the files were taken to the Office of the DPP (Director of Public Prosecution). The Resident State Attorney in Tororo advised that the matter be handled administratively.”
Delays in receiving adequate treatment at health facilities increase the risk of maternal death. These delays are caused by shortages of medical supplies, equipment and adequately trained health workers, which undermines the timeliness and quality of medical care available to expectant mothers.
The delays Odoi experienced at Tororo hospital is a symptom of the fragility of the public health system in a country where there is one employed skilled health professional for every 1,000 persons.
This has forced some expectant mothers to seek services away from government facilities.
Tororo hospital has one operating theatre with two rooms.
“In November 2022, I was in labour and went to the hospital and they asked for Shs300,000. I told them that I had Shs200,000. This was for a caesarean section operation. I ran from the hospital and found a traditional birth attendant and she helped me deliver at Shs50,000,” a mother, who spoke on condition of anonymity, says.
Declining health budgets have led to a cyclical crisis peppered with acute staffing shortages, apathy and despondency among poorly paid medical staff.

Mr Francis Odoi, a resident of Nyakesi Zone “A” in Nyangole Sub-County, Tororo District. Mr Odoi blames negligence of health workers at Tororo General Hospital for the death of his wife. Photo | Yahudu Kitunzi
George Olowo, the LC3 Chairperson of Nyangole Sub-county, recounts his wife’s experience at the hands of some medical workers at Tororo Hospital.
“My own wife went to the hospital to give birth. She carried everything, the polythene, the mama kit and money. After giving the nurse money, the nurse disappeared,” he says.
This experience is echoed by Peter Okoth, a resident of Nyakesi of Zone A in Nyangole Sub-county. According to him, the practice of soliciting bribes and extorting from vulnerable patients is rife in the facility.
Okoth recounts how he only received treatment and care for his pregnant wife after parting with money.
“I received a call from my sister around midday and she said there was a nurse saying the child was not seated well in the womb and she needed an injection. I knew what the nurse was talking about. Then I asked my sister to ask the nurse, how much she wants,” he says.
Bribing health workers for services at health facilities is common in Uganda.
On average, households pay Shs106,000 in bribes to access health care, according to a 2021 study by the Inspectorate of Government. Typically, those who needed maternal services were asked to pay Shs15,000.
Juliet Ayo, a human rights activist in Tororo, says the situation is dire for those in the lowest rungs of society.
“We advocated for the doctors and nurses to wear name tags so that when someone is asking you for money you can’t afford and you are reporting them to our office, you are able to identify them. But they are not reporting these cases to us. I have a case in court where we sued the hospital for rash and negligence. The nurse missed a vein on a boy’s hand and they had to amputate the hand,” she says
Simon Peter Okongo, the LC1 Chairperson for Nyake Central, says this creates a situation where both the giver and receiver are guilty of corruption.
Critically, staffing norms in public health facilities in Uganda have not been adjusted in light of a growing population, increasing the likelihood that staff are overworked.
In this context, government efforts to increase the uptake of maternal health service in public facilities is undermined.
Dr Okoth Obbo, the Tororo District health officer, says: “I cannot confirm or deny that maternal death at our facilities may repel or discourage mothers from giving birth in our facilities. But these deaths are not on a daily basis, they are once in a while and we have realised some of the mistakes were from us and others from the mothers themselves.”
He adds: For example, a mother comes in and we take her details but when it is time to deliver, she is nowhere to be found. They have either stepped out briefly or discharged themselves. We suspect they go to traditional birth attendants, where they are given herbs to take to speed up the process. But by the time they return to the hospital, they are in a bad state and that can lead to maternal death.”
He further says: “Some of these deaths are inevitable, others are due to mistakes that we learn from. If there are issues with our staff, we encourage them to tell us or in confidence, we are willing to listen.”
Dr Obbo also says there are other factors such as the distance from the expectant mother’s home to the health centre that hinder the delivery of services.
“Because of distance, it hinders their uptake of these maternal health services. So, they either deliver with the help of traditional birth attendants or they deliver from home. Expectant mothers prefer traditional birth attendants to our mid-wives because for them they have a personal touch. Their customer care seems to be better than ours because our midwives are overwhelmed, they have a lot of work they do not give personal attention to these mothers and yet they need one on one care.”
Investment in the health sector has mirrored the trend of health-seeking behaviour as more people seek services in the private health facilities. The government has prioritised investment in private health services such as the Lubowa hospital where the government doled out $379.71 million (Shs1.4 trillion) on the project.
The situation at Tororo General Hospital, like elsewhere, sharply contrasts the pristine first world hospitals where the political elite, their children and friends are flown to receive treatment on taxpayer funds, a practice akin to medical apartheid. It is a practice that public watchdog organisations are demanding, must stop.
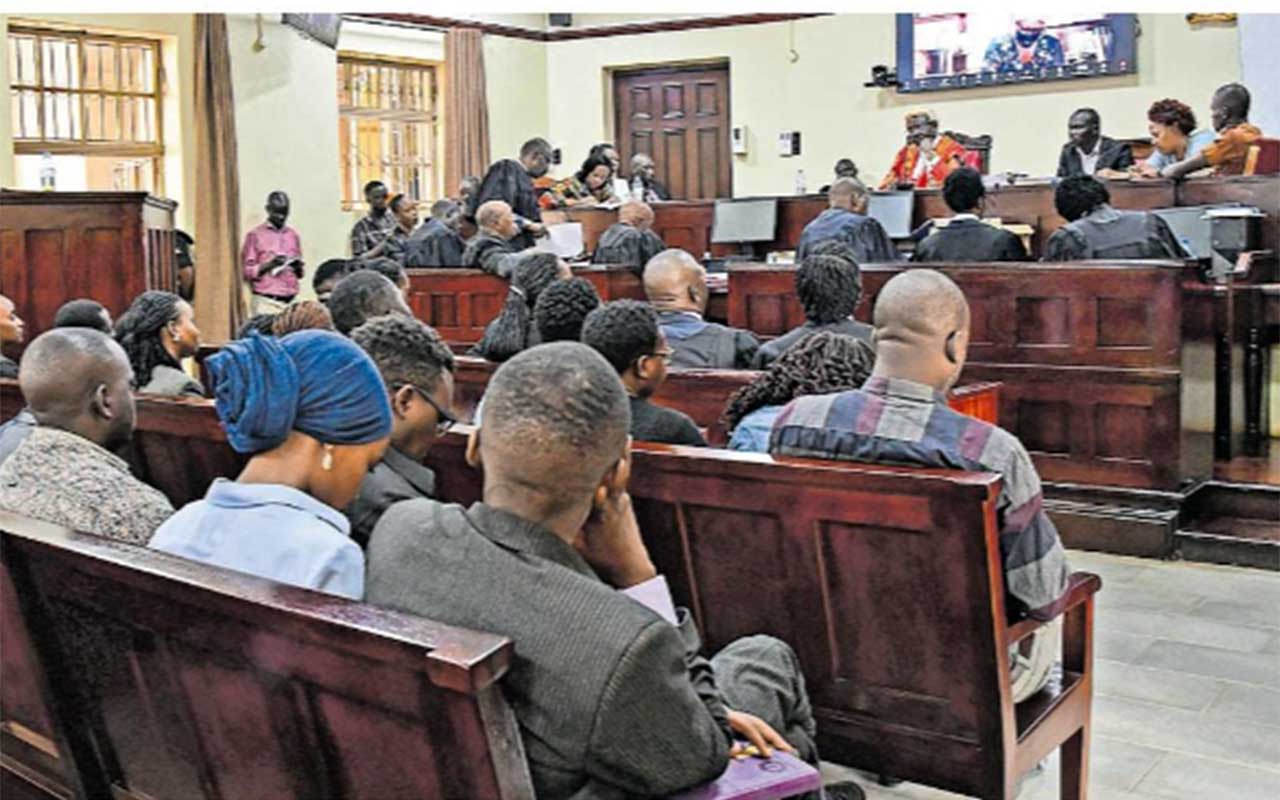
Court
A 2020 Supreme Court judgement found that the government’s failure to provide health care for expectant mothers was a violation of their right to health and unconstitutional.
The court also found that the government’s failure to provide emergency services to expectant mothers in public health facilities resulting in their injury and inhumane treatment is unconstitutional.
Court instructed the government to provide sufficient funds in the budget for maternal healthcare. This landmark ruling set a precedent as it arose from a lawsuit against the government following the death of two expectant mothers; Rhoda Kukiriza and Inziku Valente.
Steven Masiga, a researcher, cites these legal precedents when proposing remedies.
“We encourage those aggrieved by the inefficiencies of the health workers in Tororo to take them on legally. Once you have duty of care, you have a duty imposed on you by law and you fail to execute that duty. It is an offence,” Masiga told this publication.
“When trying cases where medical workers are charged with rash and negligent acts causing death, courts in Uganda typically make judgements based on the evidence from post mortems for example, that prove the cause of death was due to the rash actions or negligence of the medical worker in question,” he adds.
This provides no solace for Ochieng and Odoi who may not have means to hire a lawyer or understand the procedures to file a complaint before the Uganda Medical and Dental Practitioners Council which will then sit and determine whether to sanction an inquiry.