Prime
3 years of grappling with cervical cancer

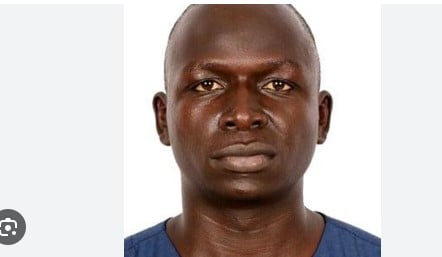
Ms Ziyada Muwugumya after undergoing cervical cancer screening at Kibuku Health Centre. PHOTO/MUDANGHA KOLYANGHA
What you need to know:
Cancer prevalence
- According to figures of 2018 Uganda Cancer Organisations and Resources data, about 17.8 per cent of the population are at risk of getting cancer.
- The country registers about 60,000 cases of cancer per year and 22,000 of these die every year. It is estimated that in the next 10 years, cancer cases in the country will grow to 80,000 per year.
- The Uganda Cancer institute (UCI) also indicates that about 80 per cent of the cases of cancer are presented in their advanced stages making it hard for any of these to be reversed.
Because she did not get early cancer diagnosis, Ms Zyada Muwugumya, 39, has been wallowing in pain for close to three years now.
Ms Muwugumya, who hails from Bukatikoko Village in Kibuku Town Council, says cervical cancer comes with pain and stigma. She adds that her life has continued to deteriorate despite the treatment.
“I was a productive farmer but this problem has left me more crippled. I am doing nothing to sustain my family. The children need money for school fees but part of my body is completely weak,” she says.
Ms Muwugumya is married with five children.
After two years of pain and uncertainty, Ms Muwugumya was brought to light in 2017, after a team of qualified personnel carried out a health camp in the district, including cancer screening and diagnosed her with cervical cancer.
“Messages of cancer were spread in the district and I took up that advantage only to be told that the pain was a result of cervical cancer. The pain that I was undergoing was extremely high and yet I had no money to visit health units,” she said.
“As you (can) see, I am feeling too much pain even in the private parts but the most disturbing part is that my husband still wants sex. This is quite terrible,” she adds.
Ms Muwugumya says she has been battling with the cancer for the last three years and she has no money to go to hospitals.
“Attempts to move from one health centre to another is compounded with lack of specialised doctors and drugs which we are told to buy and they too are expensive,” she notes
Ms Muwugumya has thought of committing suicide but neighbours gave her words of encouragement.
“The biggest challenge, that is likely to cause my death is lack of money for treatment. Every health facility that I attempt to seek medication from, demands for money, which I don’t have. I have left it in the hands of God,” she said.
Experts say
The number of patients suffering from cervical cancer seems to be high, coupled with lack of proper medical facilities. “The challenge is that most women don’t seek treatment early enough and only turn up when the situation has worsened. Lack of information to the mothers is another factor,” Dr Ahamed Bumba, a senior health officer, said.
Mr Alifa Amuza Dankaine, the focal person of Uganda Cancer Research Foundation, says after assessment last month at a camp in Kibuku District, it was discovered that more cases were being registered following community sensitisation.
Fifteen women suspected to have cervical cancer were detected and referred to Mbale hospital.
“We are indeed concerned over the alarming levels of cancer-related cases in the district. At least 15 patients have been diagnosed and confirmed to be suffering from this problem with many cases being registered deep in the rural villages,” Mr Dankaine said.
He added: “Most patients are suffering because of ignorance about the symptoms of the cancer and yet it looks as if it is a neglected disease but slowly killing people because they take a long period to detect the disease in its early stages”.
Mr Dankaine says the district is being taken by surprise at the upsurge of the disease.
He, however, says they have been sensitising local communities on the current wave of cancer.
But while some people are more likely to get cancer, their chances of survival can be minimised if they seek early diagnosis. Health experts say all sexually active women in their reproductive age are potential victims of cervical cancer disease.
Dr Kenneth Mugabe, a gynaecologist at Mbale hospital, says the facility has the ability to effectively attend to this type of cancer but only when it is detected early.
Cervical cancer is acquired when a woman gets exposed to the human papilloma Virus [HPV], in her reproductive system particularly on the outer part of the cervix.
“As the infection spreads, it causes abnormal tissue growth and other changes to cells within the victim’s cervix,” Dr Mugabe says.
He adds that since the virus is sexually transmitted, many women can survive with it for a year and if undetected, itw eventually leads to conversion of abnormal cells on the surface of the cervix.
“We usually encourage all women of reproductive age to turn up for cervical screening services such that they know their status and seek treatment before it is too late,” he said.

Residents attend a sensitisation camp on cancer, diabetes and high blood pressure in Mityana District in 2015. Experts encourage sensitisation for early detection of cancer. PHOTO/FILE
Dr Mugabe says the signs one should get suspicious of are constant bleeding, and foul vaginal discharge
He, however, adds that many victims tend to ignore these signs until the late stages when they start feeling abdominal pain, difficulty in passing urine or when they experience weight loss and general body weakness. This type of cancer [Cervical] has a close link to HIV/Aids and infected mothers are more susceptible.
“The process of screening is a simple exercise that the victims should not fear to undertake. It requires a few minutes and it is done by visual inspection and treatment is available at no cost in public health facilities,” he explains.
Dr Simon Mbulayiteye, a researcher and cancer specialist based in America, had earlier told Daily Monitor that cancer is another disease that has been neglected mostly in Uganda.
“People are quietly being killed by cancer without noticing because government pays little attention to scale down this deadly disease. For every 100 people, 30 of them have cancer problems in the country,” Dr Mbulayiteye says.
According to the world cancer report, with the existing knowledge, it is possible to prevent at least one third of the 10 million cancer cases that occur each year in the world.
“By the end of 2020, there will be a 50 per cent increase in the number of people diagnosed with cancer unless steps are taken now,” Dr Mbulayiteye warns.
He adds that a third of the population can be rescued through lifestyle change.
“Lack of specialised doctors to deal firmly with cancer is yet another challenge and soon, the district would be taken by surprise due to the upsurge of cancer cases. This will definitely also leave the entire population poor because they will no-longer be productive,” Dr Mbulayiteye says.
He called for more community awareness and early diagnosis for people in rural areas.Dr Mbulayiteye notes that most cancer cases are those of cervical and breast.
Cervical cancer screening and awareness
The best way to protect yourself from cervical cancer is by attending cervical screening.
Women aged 25 to 49 are offered screening every 3 years, and those aged 50 to 64 are offered screening every 5 years.
During cervical screening, a small sample of cells is taken from the cervix and checked under a microscope for abnormalities.
In some areas, the screening sample is first checked for human papillomavirus (HPV), the virus that can cause abnormal cells.
Using condoms during sex offers some protection against HPV, but it cannot always prevent infection because the virus is also spread through skin-to-skin contact of the wider genital area.
The HPV vaccine has been routinely offered to girls aged 12 and 13 since 2008.
If cervical cancer is diagnosed at an early stage, it’s usually possible to treat it using surgery. In some cases, it’s possible to leave the womb in place, but it may need to be removed.
Cervical cancer is the commonest in women and among all the others in Uganda. It is one of the preventable cancers because of the Human Papilloma Virus (HPV) vaccine. New cases of cervical cancer as of 2018 were 6,413, and the number of deaths stood at 4,301.